This section contains a background to Cow's Milk Allergy (CMA). It provides information on managing CMA by appropriate assessment and diagnosis according to relevant guidelines, and advice on when to use an amino acid-based formula for infants and children with CMA.
CMA Overview
CMA is a distressing condition for infants and their parents/carers:
- CMA is an immune mediated reaction to the proteins within cow's milk and is one of the most common food allergies affecting 2-5% of infants.1 Up to 40 000 babies a year in the UK may develop CMA.2
- Most cases of CMA present in infancy and the majority of children will grow out of the allergy by the age of 5 years.
- CMA can be complex to diagnose as many infants will often present with two or more symptoms frequently seen in infancy.
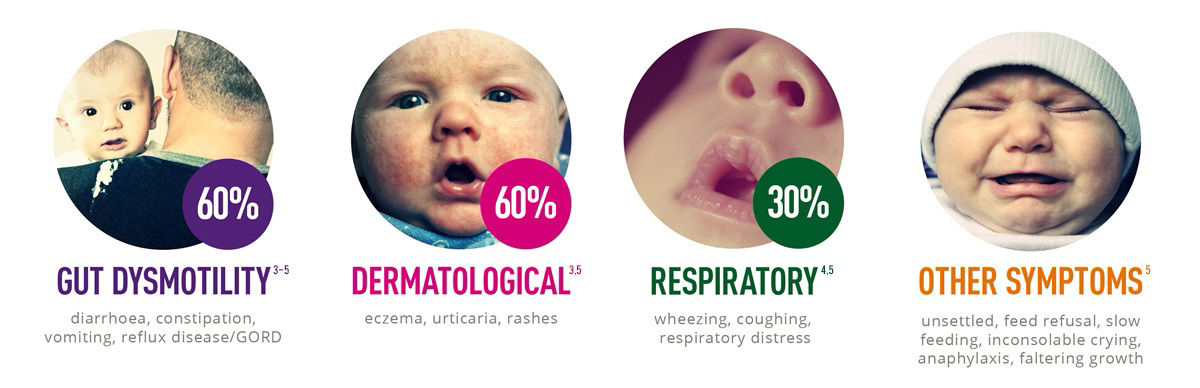
- The most common symptoms are of dermatological, gastrointestinal and respiratory origin.
Symptom complexity can delay diagnosis
Data from the UK shows:6
- It takes an average of 3.6 months from initial GP visit to formal diagnosis
Delayed diagnosis prolongs the distress for infants and their parents and has the potential to impact on infants' growth and development.
CMA imposes a substantial burden on the NHS
Patients with CMA had a mean of 18.2 clinician visits and cost the NHS an estimated £25.6 million during the first 12 months after initial presentation:6
The initial aim of management is prompt and accurate diagnosis, removal of cow's milk protein from the diet whilst ensuring the nutritional requirements of the infant/child are met using suitable specialist formulas and dietary modification.
- Fiocchi A, Brozek J, Schünemann H, et al. WAO J 2010;3:57-161
- 2011/12 UK Birth Rate, Office of National Statistics, ONS http://www.ons.gov.uk/ons/taxonomy/index.html?nscl=Population Number of births in UK 2012 = 812,970
- Meyer R, Schwarz, C & Shah, N. Current Allergy & Clinical Immunology 2012;25(1):10-17.
- Høst A. Ann Allergy Asthma Immunol 2002;89 (6 suppl 1):33-37.
- Koletzko S, Niggemann B, Arato A, et al. J Pediatr Gastroenterol Nutr 2012; 55(2):221-229.
- Sladkevicius E, Nagy E, Lack G et al. Resource implications and budget impact of managing cow milk allergy in the UK. J Med Econ 2010;13(1):119-28.
CMA assessment
NICE have produced a guideline (CG 116) to aid in the diagnosis and assessment of food allergy in children and young adults. The first steps are initial recognition, an assessment of the symptoms and the allergy focused history. The guideline includes a series of algorithms, which have been reproduced with the permission of NICE for use on this website.
Consider Food Allergy in a child or young person who:
- has one or more signs and symptoms of possible food allergy (pay particular attention to persistent symptoms that involve different organ systems) or
- has had treatment for atopic eczema, gastro-oesophageal reflux disease or chronic gastrointestinal symptoms (including chronic constipation) but their symptoms have not responded adequately.
Do not offer allergy tests without first taking an allergy-focused clinical history.
A healthcare professional with the appropriate competencies (a GP or other healthcare professional) should take an allergy-focused clinical history tailored to the presenting symptoms and age of the child or young person using the questions below.
The clinical history should include:
- any personal history of atopic disease (asthma, eczema or allergic rhinitis)
- any individual and family history of atopic disease (asthma, eczema or allergic rhinitis) or food allergy in parents or siblings
- details of any foods that are avoided and why
- an assessment of presenting symptoms and other symptoms that may be associated with food allergy, including:
- age at first onset
- speed of onset
- duration, severity and frequency
- setting of reaction (for example, at school or home)
- reproducibility of symptoms on repeated exposure
- what food and how much exposure to it causes a reaction
- cultural and religious factors that affect the child's diet
- who has raised the concern and suspects the food allergy
- what the suspected allergen is
- the child's feeding history, including age of weaning and whether they were breastfed or formula-fed (if the child is currently being breastfed, consider the mother's diet)
- details of previous treatment, including medication, for the presenting symptoms, and the response to this
- any response to the elimination and reintroduction of foods
- physical Examination
- Based on the clinical history, physically examine the child or young person, paying particular attention to:
- growth and physical signs of malnutrition
- signs indicating allergy-related comorbidities (atopic eczema, asthma and allergic rhinitis)
Based on the allergy-focused clinical history, consider referral to secondary or specialist care in any of the following circumstances.
The child or young person has:
- faltering growth in combination with one or more of the gastrointestinal symptoms described in signs and symptoms of possible food allergy
- not responded to a single-allergen elimination diet
- had one or more acute systemic reactions
- had one or more severe delayed reactions
- confirmed IgE-mediated food allergy and concurrent asthma
- significant atopic eczema where multiple or cross-reactive food allergies are suspected by the parent or carer
There is:
- persisting parental suspicion of food allergy (especially in children or young people with difficult or perplexing symptoms) despite a lack of supporting history
- strong clinical suspicion of IgE-mediated food allergy but allergy test results are negative
- clinical suspicion of multiple food allergies
National Institute for Health and Care Excellence (2011) Adapted from CG 116 Food allergy in children and young people. Diagnosis and assessment of food allergy in children and young people in primary care and community setting. London: NICE. Available from www.nice.org.uk/CG116 Reproduced with permission.
Diagnosis
CMA can be classified according to whether the allergic reaction is an IgE mediated (within 2 hours) or a non IgE mediated (delayed, chronic) response. The NICE guideline helps determine the type of allergy and outlines the tests that should be used to confirm the diagnosis.
Once an allergy is suspected NICE recommends that an elimination diet should be tried for 2 to 6 weeks. The allergen should then be reintroduced to confirm diagnosis. NICE also recommends that the advice of a dietitian with appropriate competencies should be sought to assist with nutritional adequacies, timings of elimination and reintroduction, and follow-up.
The algorithms found below have been reproduced with the permission of NICE.
Once the diagnosis of the CMA has been confirmed, including the type of allergy (IgE or non IgE), a management plan can be established.
Alternative diagnostic tools not recommended.
Do not use the following alternative diagnostic tests in the diagnosis of food allergy:
- vega test
- applied kinesiology
- hair analysis
Do not use serum-specific IgG testing to diagnose food allergy.
Offer a skin prick test and/or blood tests for specific IgE antibodies to the suspected foods and likely co-allergens.
Base choice of test on:
- the clinical history and
- the suitability, safety for, and acceptability to the child or young person (or their parent or carer) and
- the available competencies of the healthcare professional to undertake the test and interpret the results
Tests should only be undertaken by healthcare professionals with the appropriate competencies to select, perform and interpret them.
Only undertake skin prick tests where there are facilities to deal with an anaphylactic reaction.
Interpret test results in the context of clinical history.
Do not use atopy patch testing or oral food challenges to diagnose IgE-mediated allergy in primary care or community settings.
Try eliminating the suspected allergen (normally for between 2-6 weeks), then reintroduce. Seek advice from a dietitian with appropriate competencies about nutritional adequacies, timings of elimination and reintroduction, and follow-up.
Taking into account socioeconomic, cultural and religious issues, offer information on:
- what foods and drinks to avoid
- how to interpret food labels
- alternative sources of nutrition to ensure adequate nutritional intake
- the duration, safety and limitations of an elimination diet
- oral food challenge or reintroduction procedures, if appropriate, and their safety and limitations
If allergy to cow's milk protein is suspected, offer:
- food avoidance advice to breastfeeding mothers
- information on appropriate hypoallergenic formula or milk substitute to mothers of formula-fed babies
Seek advice from a dietitian with appropriate competencies.
Based on the allergy-focused clinical history, consider referral to secondary or specialist care in any of the following circumstances.
The child or young person has:
- faltering growth in combination with one or more of the gastrointestinal symptoms described in signs and symptoms of possible food allergy
- not responded to a single-allergen elimination diet
- had one or more acute systemic reactions
- had one or more severe delayed reactions
- confirmed IgE-mediated food allergy and concurrent asthma
- significant atopic eczema where multiple or cross-reactive food allergies are suspected by the parent or carer
There is:
- persisting parental suspicion of food allergy (especially in children or young people with difficult or perplexing symptoms) despite a lack of supporting history
- strong clinical suspicion of IgE-mediated food allergy but allergy test results are negative
- clinical suspicion of multiple food allergies
National Institute for Health and Care Excellence (2011) Adapted from CG 116 Food allergy in children and young people. Diagnosis and assessment of food allergy in children and young people in primary care and community setting. London: NICE. Available from www.nice.org.uk/CG116 Reproduced with permission.
Management
CMA is managed by excluding cow's milk protein from the diet.
Breast feeding is always the preferred way to feed an infant. If an infant is being breast fed, the mother needs to follow an exclusion diet with the support of the dietitian to ensure that the maternal diet is adequate. Calcium and Vitamin D supplements are recommended.
Formula fed infants will need to be provided with a replacement hypoallergenic formula, either an extensively hydrolysed or amino acid formula.
There are specific times where the use of an amino acid formula is indicated.


- Meyer R et al. J Allergy Clin Immunol Pract. 2017.09.003
- Fox et al. Clin Transl Allergy (2019); 9: 40
- Luyt et al. Clin Experimental Allergy;44:642-672

