The term FGID refers to a group of recurring symptoms and feeding problems known as Functional Gastrointestinal Disorders. Managing the symptoms of FGIDs can be challenging. We’ve gathered the latest guidelines and expert opinions to support healthcare professionals to make the correct diagnosis and help to reduce concern among parents.
The symptoms of FGIDs can cause discomfort for an infant and huge amounts of stress for parents. Once satisfied the infant has no serious underlying disease, there are a number of ways healthcare professionals can approach the problem, ensuring any intervention plan attends to both the infant and the family1, these include:
- Parental reassurance and support
- Practical management
- Nutritional management
- Medical management
Parental Reassurance and Support
First and foremost, parents need support. It is important to consider that concerns about FGIDs are not only about the infant’s symptoms, but also about the family’s wellbeing. It is necessary to, not only make a diagnosis, but also recognise the impact of the symptom(s) on the family’s emotions and ability to function1.
Once you have reassured the parents, practical tips and advice can help, such as teaching appropriate responses to their infants, more effective soothing, and where appropriate, reviewing their feeding practices2-3.
Practical tips for managing reflux and regurgitation4
- Avoid overfeeding – try feeding smaller amounts more frequently
- Feed the infant in an upright position
- Burp the infant frequently before, during and after feeding
- If the infant is bottle fed, check the hole in the teat is not too large – this can cause infants to gulp their feed too quickly
Practical tips for managing colic5-6
- Gentle motion (for example pushing the pram and rocking the crib)
- ‘White noise’ (for example from a vacuum cleaner, hairdryer or running water)
- Bathing the infant in a warm bath
- Preventing the infant from swallowing air by sitting them upright during feeding
- Minimising stimulation by placing the infant in a quiet environment
Parents should be encouraged to look after their own well-being by5:
- Resting when possible
- Asking family and friends for support
- Meeting other parents with infants of the same age
Practical tips for managing functional constipation
- Give extra cooled boiled water between normal feeds7
- If using infant formula, ensure it is made up exactly as directed by the manufacturer and not diluted or over-concentrated
- Gently move infant’s legs in a bicycling motion, or carefully massage their tummy to help stimulate their bowels
- Giving a warm bath may help
Nutritional management
Breastfeeding is the best source of nutrition for infants and provides many benefits8. In managing digestive problems in infants, it is important to avoid the use of drugs and invasive procedures where possible. Nutritional management is generally the preferred option9.
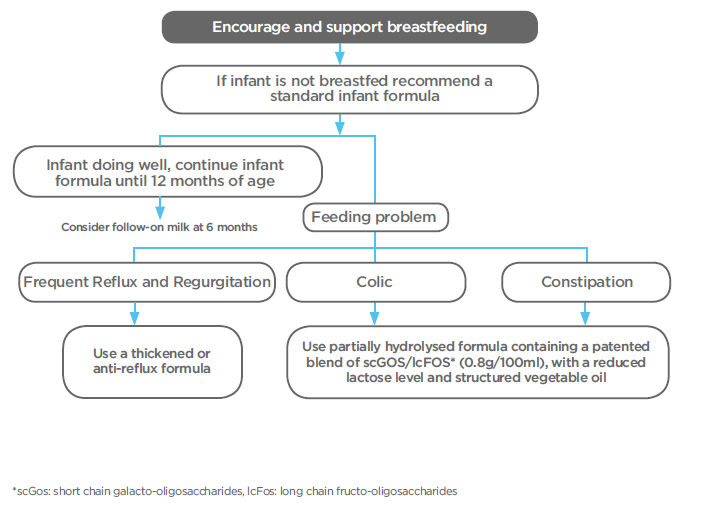
Medical management can be considered as an option if nutritional management does not suffice.
- Hyman PE et al. Gastroenterology 2006; 130: 1519-1526.
- Savino F. Acta Paediatr 2007; 96: 1259-1264
- Owens C et al. SA Pharmaceutical Journal 2013; 80(3): 28-30.
- NICE. NG1. Gastro-oesophageal reflux disease: recognition, diagnosis and management in children and young people. 2015.
- NICE Clinical Knowledge Summary. Colic.
- NHS Choices. Colic. 2012.
- NHS Choices. Constipation and soiling in children.
- Horta BL et al. Food Dig 2012; 3: 63-77
- Vandenplas Y et al. Essential Knowledge Briefing. Wiley Chichester (2015)

