Better nutrition, better outcomes
Nutrition is important at every stage of the life cycle, and both during times of health and disease or illness. Ensuring that patients are meeting their nutritional needs is an important part of their overall care and can help to support positive clinical outcomes.
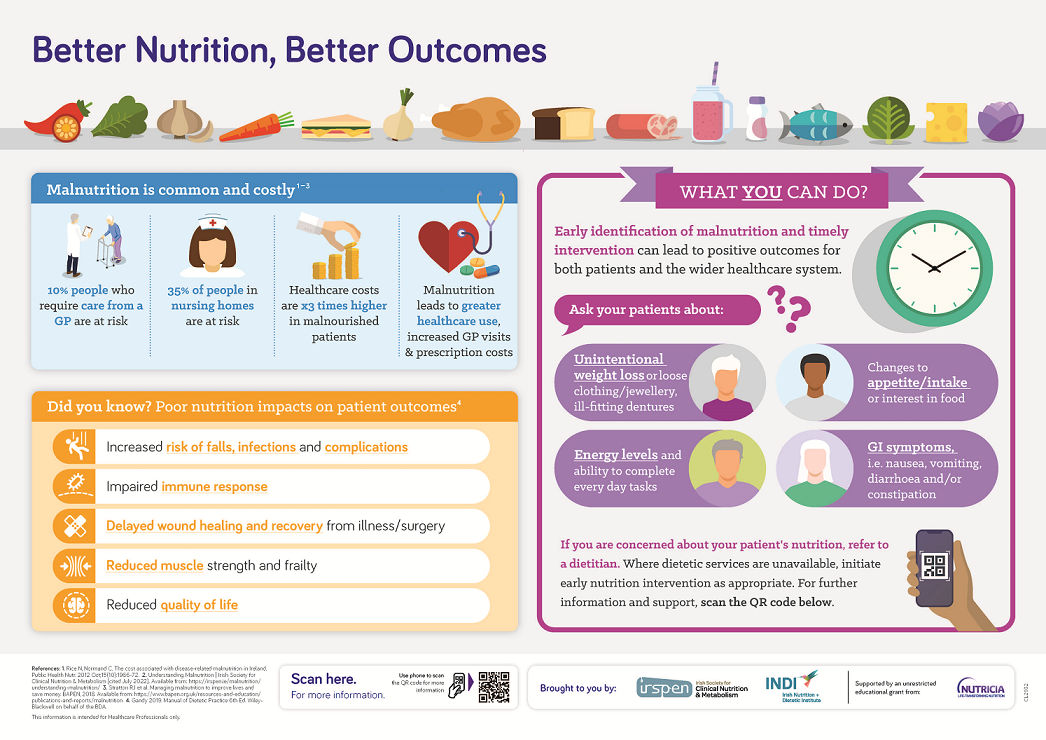
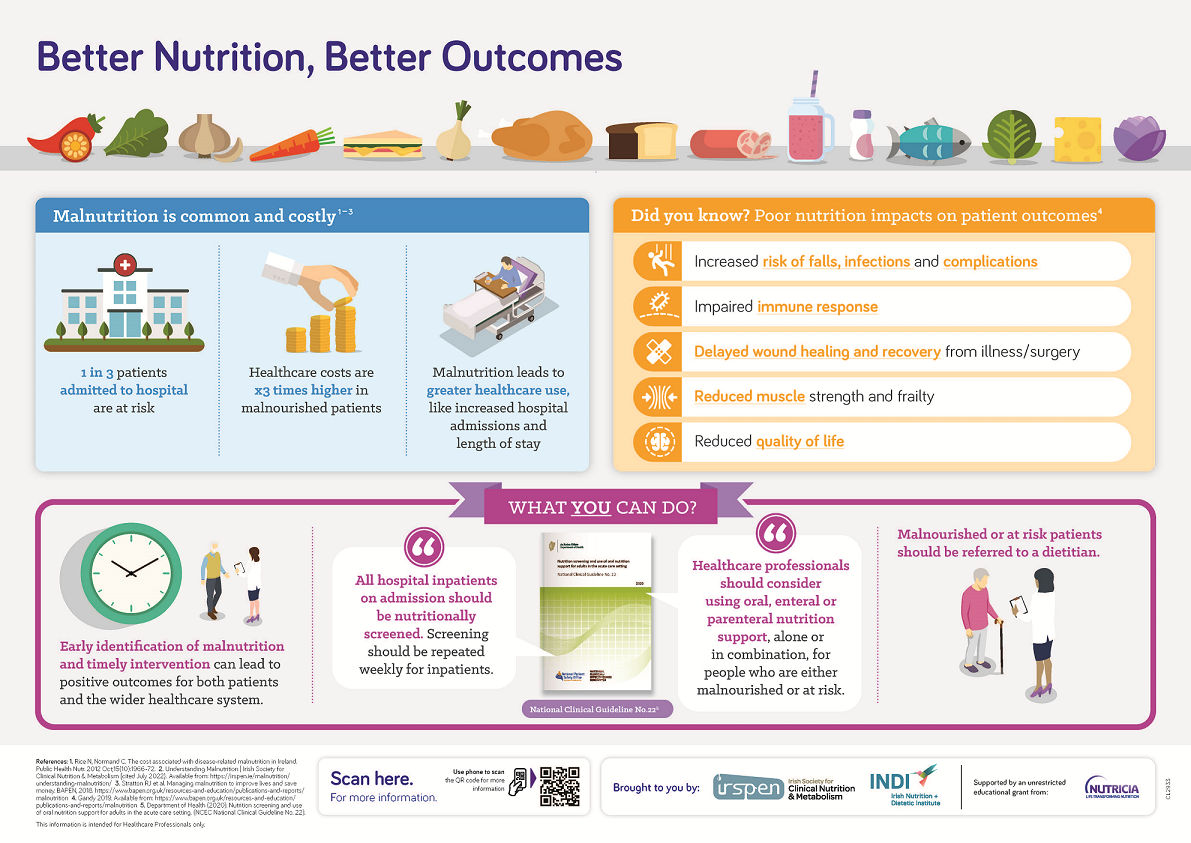
Poor nutrition can greatly impact a patient’s clinical outcomes. Those who are malnourished are at risk of1,2:
- Increased falls, infections and complications
- Impaired immune response
- Delayed wound healing and recovery from illness/surger
- Reduced muscle strength and frailty
- Reduced quality of life and psychosocial function
Malnutrition is common and costly3-5
At any one time in Ireland, malnutrition affects approximately 145,000 adults. While 1 in 3 patients admitted to hospital are at risk of malnutrition, over 95% of malnourished people are community based. Around 10% of people who require care from a GP are at risk and 35% of people in nursing homes are also at risk.
Healthcare costs associated with malnutrition exceed those of obesity. Malnutrition leads to greater healthcare use, for example increased hospital admissions and length of stay, increased GP visits and increased prescription costs. Overall, healthcare costs are x3 times higher in malnourished patients than in those who are not malnourished.
As outlined above, malnutrition may be more common than you think, with 1 in every 10 people walking through the doors of a GP practice at risk. While anyone can be at risk, there are some groups who are at higher risk of becoming malnourished:
- 65 years or older
- Living with a long-term health condition (for example lung disease)
- Living with cancer
- Experiencing difficulties swallowing
- Living alone
It’s important to remember that people who are overweight or obese can also be at risk of malnutrition. Use of a nutrition screening tool will help you to identify patients who are either malnourished or at risk of becoming malnourished. Read on for further information on nutrition screening.
Nutrition screening is used to identify people or patients who are either already malnourished or at risk of becoming malnourished. Many validated screening tools exist, however the most commonly used tools in Ireland are the Malnutrition Universal Screening Tool (MUST) and the Malnutrition Screening Tool (MST). Both of the above screening tools are quick and easy to use.
National Clinical Guideline No. 22, published by the Department of Health in 2020, outlines the requirements for nutrition screening and intervention in the adult acute care setting. The guideline states that “all hospital inpatients on admission should be screened. Screening should be repeated weekly for inpatients” and that “healthcare professionals should consider using oral, enteral or parenteral nutrition support, alone or in combination, for people who are either malnourished or at risk”.
Access the full guideline or a summary document here: Nutrition screening and use of oral nutrition support for adults in the acute care setting
Nutrition screening in the community is also important, given that over 95% over those who are malnourished are community based. It is recommended that screening in the community be completed opportunistically (e.g. on first contact within a new care setting) and upon clinical concern (e.g. if a person shows signs of unplanned weight loss, reduced physical function, etc. See below for more on this).2 At risk groups, such as those living in care home settings, as well as those identified as either malnourished or at risk of becoming malnourished should be screened more frequently (e.g. monthly).
Managing malnutrition is everyone’s responsibility. The first step is to start the conversation with your patients about their nutrition. Ask your patients about:
- Unintentional weight loss or loose clothing/jewellery, ill-fitting dentures
- Energy levels and ability to complete every day tasks
- Changes to appetite/intake or interest in food
- GI symptoms, i.e. nausea, vomiting, diarrhoea and/or constipation
It is important that once a person has been identified as either malnourished or at risk of becoming malnourished, that immediate action is taken. Early identification of malnutrition and timely intervention can lead to positive outcomes for both patients and the wider healthcare system.
If you are concerned about your patient’s nutrition, refer to a dietitian. Where dietetic services are unavailable, initiate early nutrition intervention as appropriate. Nutrition intervention may include dietary advice and/or oral nutritional supplements. Download our patient information booklet below and read on for more information on oral nutritional supplements.
Oral Nutritional Supplements (ONS) are drinks containing a concentrated source of energy, protein, vitamins and minerals and are an evidence-based strategy for the dietary management of disease related malnutrition. ONS are indicated when a patient is unable to meet their nutritional requirements through diet alone and where oral intake is safe.
What are the clinical benefits of ONS?2, 6-11
- Improvements in:
- Nutrient intakes (without suppression of appetite)
- Weight
- Hand grip strength (indicating functional status)
- Quality of life
Reductions in:
- Complications (e.g. infections, pressure ulcers, poor wound healing)
- Hospital admissions & readmissions
- Length of hospital stay
- Mortality
ONS come in many different flavours, styles and sizes. The evidence base for ONS is largely in ready to drink ONS prescribed for a mean period of approximately 3 months, vs dietary control.
ONS are not designed as a meal replacement and should always be taken in addition to meals and snacks. For more information and to explore our range of ONS, please click here: Adult Oral Range
Should you wish to speak to our team about any of the above information or any of the Nutricia range of products, please contact us on: support.ireland@nutricia.com or 1800 412 414.
- Gandy 2019. Manual of Dietetic Practice 6th Ed. Wiley-Blackwell on behalf of the BDA.
- A Guide to Managing Adult Malnutrition in the Community Pathway. Available from: https://www.malnutritionpathway.co.uk/ [accessed September 2022]
- Rice N, Normand C. The cost associated with disease-related malnutrition in Ireland. Public Health Nutr. 2012 Oct;15(10):1966-72.
- Understanding Malnutrition | Irish Society for Clinical Nutrition & Metabolism. Available from: https://irspen.ie/malnutrition/understanding-malnutrition/ [accessed September 2022]
- Stratton RJ et al. Managing malnutrition to improve lives and save money. BAPEN, 2018. Available from: https://www.bapen.org.uk/resources-and-education/publications-and-reports/malnutrition [accessed September 2022]
- National Institute of Health and Care Excellence (NICE). Nutrition support in adults: oral nutrition support, enteral tube feeding and parenteral nutrition. Clinical Guideline 32. 2006. Available from: https://www.nice.org.uk/guidance/cg32 [accessed September 2022]
- Stratton RJ, Elia M. A review of reviews: A new look at the evidence for oral nutritional supplements in clinical practice, Clin Nutr Supp. 2, 5-23. 2007.
- Parsons EL, et al. Oral nutritional supplements in a randomised trial are more effective than dietary advice at improving quality of life in malnourished care home residents. Clin Nutr. 2017 Feb;36(1):134-142.
- Norman K, et al. Three month intervention with protein and energy rich supplements improve muscle function and quality of life in malnourished patients with non-neoplastic gastrointestinal disease -- a randomized controlled trial. Clin Nutr. 2008 Feb;27(1):48-56.
- Cawood AL, Elia M, Stratton RJ. Systematic review and meta-analysis of the effects of high protein oral nutritional supplements. Ageing Res Rev. 2012 Apr;11(2):278-96.
- Stratton RJ, Hébuterne X, Elia M. A systematic review and meta-analysis of the impact of oral nutritional supplements on hospital readmissions. Ageing Res Rev. 2013 Sep;12(4):884-97.
Nutricia offers access to a wide range of support services and resources including:
- • Our free Sampling Service to order product samples and have them sent to your patients' homes.
- • A range of CPD accredited e-learning programmes.
- • Order free paper copies of our support tools for yourself or to use with your patients.
- • Sign up to receiving marketing communications and be the first to know about our free educational events & webinars, the latest scientific research and product updates.
Help us provide information most relevant to you
Please ensure your role and areas of interest are up to date.
